A record number of babies were admitted to the neonatal unit at Armadale Kelmscott memorial hospital in July, keeping nurses on their toes. Robyn Molloy spoke to clinical nurse Leanne Howell about what it was like to work in the unit.
The maternity ward at Armadale Kelmscott memorial hospital (AKMH) handles about 200 births per month.
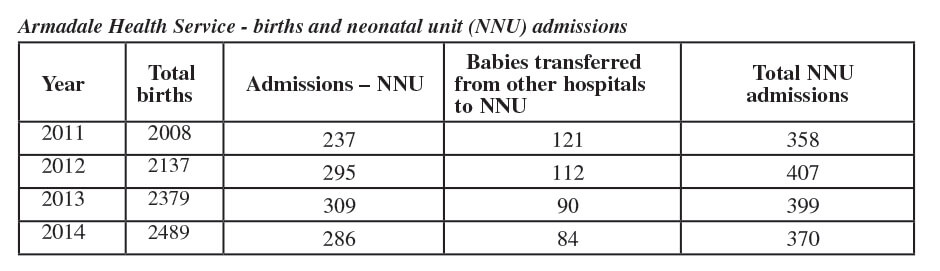
But sometimes those newborns need some extra care to kick start their lives and are admitted to the neonatal unit, usually about 30 per month.
It is a level 2a unit for sick newborns and preterm babies from 35 weeks gestation.
Services include respiratory support, intravenous therapy and naso-gastric feeding.
Babies admitted to tertiary hospitals such as King Edward can be transferred back to Kelmscott when they are well enough.
Newborns can also be stabilised in the neonatal ward prior to being transferred to tertiary care if their issues are beyond the scope of AKMH.
Clinical nurse Leanne Howell, who has been at AKMH since 2002, has been in the neonatal ward for four years and loves every minute of looking after the tiniest of patients.
She said July was the busiest month ever with 51 babies admitted to the unit, most of them coming in the first half of the month with numbers well up from the usual 35 to 40.
“Oh they are gorgeous,” she said. “They have all got their own little personalities right from the start, some are laid back and some are impatient.
“I love it down here, I have always loved little babies.
“We only have them here if they are born at 35 weeks but having said that we had one little boy who was born at 34 weeks the other day because it was too late to transfer mum.
“It it varies from baby to baby.”
Ms Howell said about 12 per cent of newborns were premature and may face a number of issues.
“If they are born early they can have issues with temperature control and may be put in the incubator,” she said.
“They may not be able to suck and have a nasal gastric tube to feed from.
“Because you don’t know why they have been born early they might have a UV antibiotic in case there is an infection there.
“We also have to monitor their blood sugar.”
Ms Howell said how long they remained in the unit depended on a number of factors as there was a ‘huge range of normal’.
Ms Howell said one of the important parts was preparing mothers to take their newborns home.
“Just before they are ready to leave we get mum to come and room in for a night or two and go through the feeding and routine before they go home,” she said.
“If we know they are going to be in for two weeks the mum will be discharged and they will come in and visit. Because they have been monitored and weighed and temperature checked, the mothers have been focused on that and so it might be nerve-racking for them to go out into the world by themselves so that is why we do that night or two.”
Ms Howell said she found the job extremely rewarding especially watching the babies get better so quickly.